Creating a diabetes diet plan involves a careful and individualized approach to ensure that the dietary recommendations effectively help manage blood sugar levels while meeting the client’s overall health needs. Here’s a step-by-step guide on how a dietician should develop a diabetes diet plan:
1. Initial Assessment and Consultation
a. Understand Medical History: Gather comprehensive information about the client’s medical history, including the type of diabetes (Type 1, Type 2, or gestational), any co-existing conditions, and current medications.
b. Assess Current Diet and Lifestyle: We Review the client’s current eating habits, food preferences, physical activity level, stress factors, and any challenges they face in managing their diet.
c. Identify Goals and Needs: Discuss and set specific, measurable, and achievable goals for blood sugar control, weight management, or other health objectives.
2. Calculate Nutritional Requirements
a. Determine Caloric Needs: Calculate the client’s daily caloric needs based on their age, gender, weight, height, and activity level.
b. Set Macronutrient Ratios: Establish appropriate macronutrient ratios for carbohydrates, proteins, and fats. For diabetes management, a common guideline is to focus on low to moderate carbohydrate intake, with a balanced distribution of proteins and healthy fats.
c. Monitor Micronutrients: Ensure the diet plan includes sufficient vitamins and minerals to support overall health, paying special attention to nutrients that may be deficient due to diabetes or medication use.
3. Develop the Diet Plan
a. Plan Balanced Meals: Create meal plans that include a variety of nutrient-dense foods. Focus on:
Low Glycemic Index (GI) Foods: Foods that have a minimal impact on blood sugar levels.
Whole Grains: Brown rice, quinoa, and whole-wheat products.
Lean Proteins: Chicken, fish, tofu, and legumes.
Healthy Fats: Avocado, nuts, seeds, and olive oil.
Non-Starchy Vegetables: Leafy greens, broccoli, bell peppers, etc.
b. Portion Control: Provide guidance on portion sizes to help manage caloric intake and maintain balanced blood sugar levels.
c. Meal Timing and Frequency: Advise on regular meal times and appropriate snack options to help stabilize blood sugar levels throughout the day.
4. Incorporate Personal Preferences and Lifestyle
a. Customize for Preferences: Take into account the client’s food preferences, cultural considerations, and any food allergies or intolerances.
b. Adapt for Lifestyle: Design the meal plan to fit the client’s daily routine, including work schedules, physical activity, and family meals.
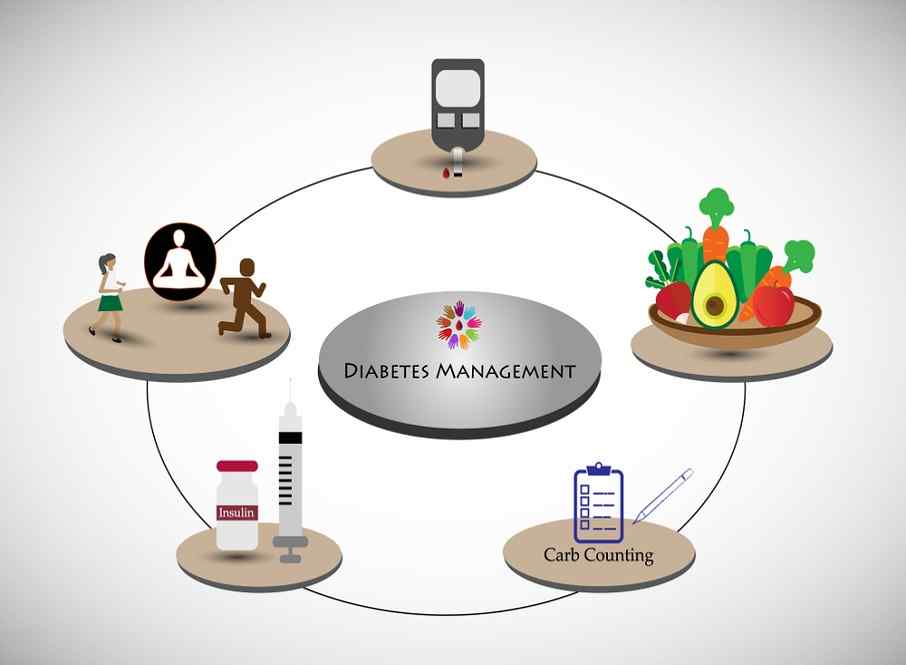
5. Education and Self-Management
a. Teach Carbohydrate Counting: Educate the client on how to count carbohydrates and understand food labels to make informed choices.
b. Provide Practical Tips: Offer practical advice on meal preparation, grocery shopping, and dining out.
c. Monitor and Adjust: Schedule regular follow-up appointments to monitor progress, address any issues, and adjust the plan as needed based on blood sugar levels and client feedback.
6. Encourage a Holistic Approach
a. Stress Management: Recommend stress-reduction techniques, as stress can affect blood sugar levels.
b. Physical Activity: Incorporate physical activity recommendations that align with the client’s fitness level and preferences.
c. Regular Monitoring: Encourage the client to regularly monitor their blood sugar levels and keep track of how different foods affect their glucose levels.
7. Document and Review
a. Create a Written Plan: Provide a detailed, written diet plan that includes meal suggestions, portion sizes, and guidelines.
b. Regular Review and Feedback: Continuously review the diet plan’s effectiveness and make adjustments based on the client’s progress and any changes in their health status.
By following these steps, I as a dietician can create a well-rounded and effective diabetes diet plan that supports the client’s health goals, promotes stable blood sugar levels, and fits their individual needs and lifestyle.